Human-Centered Health AI
Idiap Research Institute, Martigny, Switzerland

Centre du Parc,
Rue Marconi 19
CH - 1920 Martigny,
Switzerland
Our research group develops and applies artificial intelligence approaches to advance health, spanning the molecular, individual and societal scales. Our research has three main focus areas: AI for Biomolecules, AI for Evidence, and AI for Humans in Society.
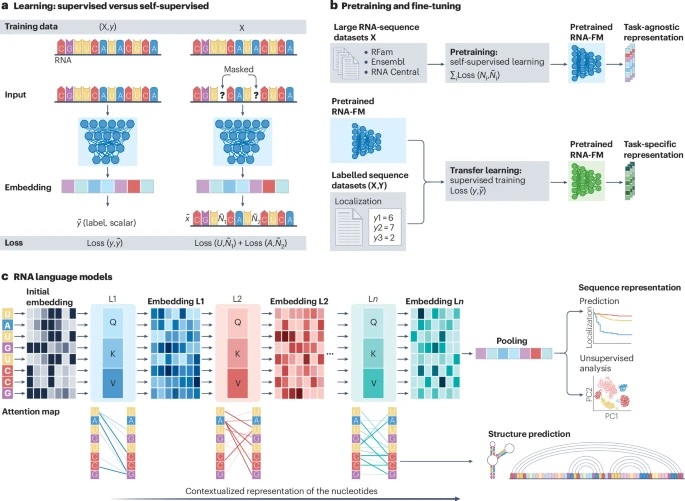
AI for Biomolecules: We develop AI approaches to understand and predict the behaviour of biological molecules, with a particular focus on small molecule metabolites and RNA. We develop and advance methods for injecting biological knowledge into molecular language models and innovate methods for interpretability and biomedical discovery based on such models. We also advance methods for using omics-data together with systems-level modelling approaches such as genome-scale models, and innovate hybrid approaches that combine data-driven with mechanistic models. Current projects within this research area include StrOntEx, MetaboLinkAI and AI4RNA.
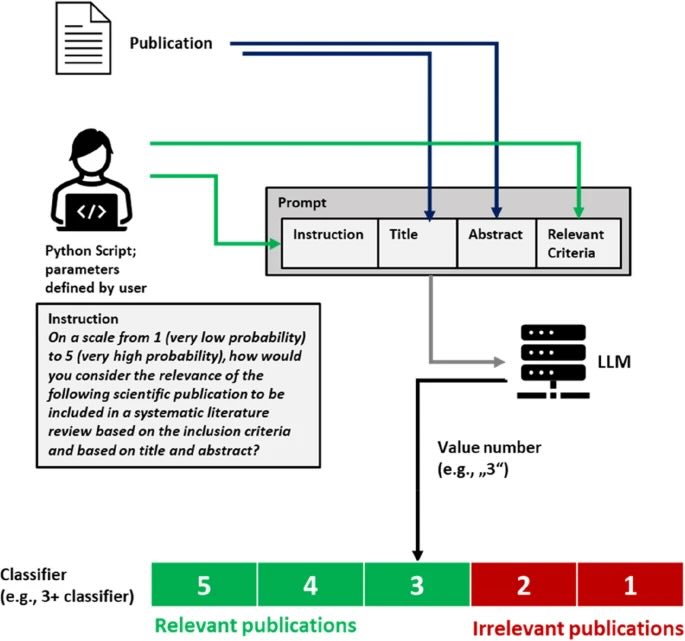
AI for Evidence: We develop AI approaches to automatically track, process, and synthesise evidence about health at scale. We aim to advance the reproducible and robust application of AI approaches in evidence synthesis and decision-making, including approaches to track evidence evolution over time, screening evidence for relevance to specific research questions, data extraction from published papers, and the automation of statistical and narrative syntheses. Current projects within this research area include GALENOS.
AI for Humans in Society investigates how modern generative AI approaches can support mental health and wellbeing, as well as the potential health risks and societal challenges that these systems might give rise to. This research examines both the opportunities and risks of deploying AI in sensitive human contexts, ensuring these technologies serve genuine human needs, and addresses how models can be improved or designed for safety and trustworthiness. Current projects within this research area include UnRealBody.