Amplifying Clinician Voices in Digital Healthcare – Exploring Human Factors and Experiences
Overview
In today’s fast-evolving healthcare landscape, digital tools have become integral to clinicians’ daily work. However, while these technologies promise to enhance efficiency and patient care, their real-world impact on healthcare professionals (HCPs) is complex and can sometimes be detrimental, leading to burnout and frustration with technology. Our project, CEDI (Clinician Experience with Digital Tools), explores this nuanced relationship by examining the daily experiences of physicians and nurses as they navigate digital transformation in hospital settings.
The Goal of CEDI
CEDI aims to explore how digitalization is reshaping the work, workflows, and professional identities of clinicians. We focus on understanding both the notable successes and persistent challenges associated with various digital tools, such as clinical information systems or electronic health records. By engaging directly with clinicians across all medical specialties and roles, we seek to uncover how these tools influence their work life, from boosting efficiency to causing daily frustrations.
Methods used
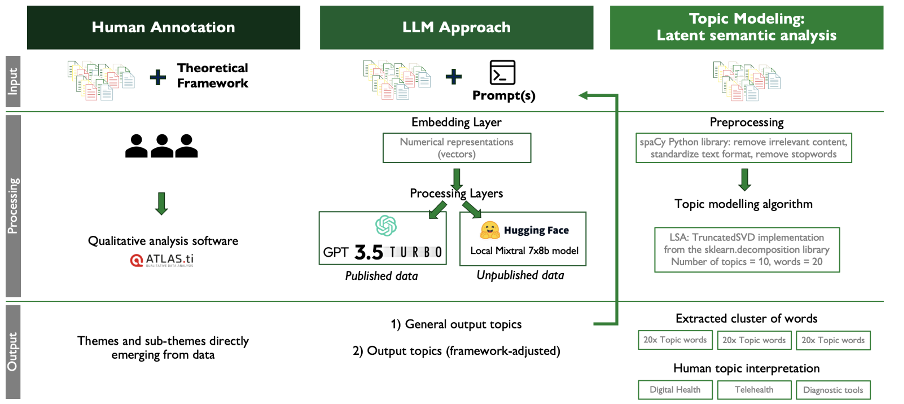
To thoroughly investigate the experiences of HCPs, we employed a multi-method approach. We conducted a systematic literature review (SLR) to synthesize existing research on HCPs’ experiences with digital tools. Next, we conducted in-depth, semi-structured interviews with clinicians in Switzerland. This phase aimed to capture their personal experiences with digital tools across various clinical roles and specialties. Finally, we explored the potential of Large Language Models (LLMs) to analyze qualitative interview data, providing insights into the interpretation of themes and topics within the data.
Sample results/Publication
Our comprehensive analysis has led to the publication of diverse and impactful findings, providing critical insights into the experiences of HCPs with digital tools:
- Experience of Health Care Professionals Using Digital Tools in the Hospital: Qualitative Systematic Review.
We identified 17 studies focusing on HCPs’ experiences with digital tools, of which 59% addressed clinical decision support tools, 35% focused on electronic health records, and 6% on remote patient-monitoring tools. We proposed a theoretical framework encompassing six constructs of positive and negative experiences, moderators, and outcomes.
Link to full publication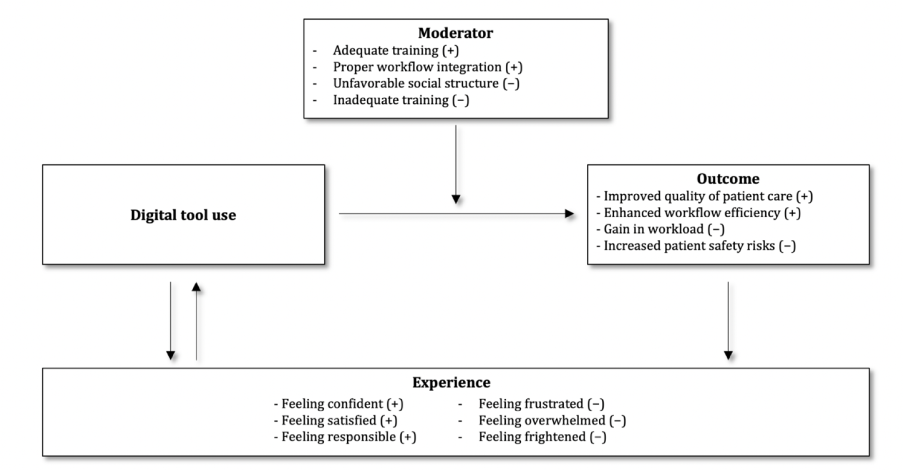
- The Paradoxes of Digital Tools in Hospitals: Qualitative Interview Study.
In this in-depth interview study with 52 healthcare professionals across 24 medical disciplines in 14 Swiss hospitals, four key themes have been revealed, namely digital tool use, workflow and processes, care delivery experiences, and digital transformation. Moreover, we uncovered six paradoxes, such as the promise of efficiency vs. the reality of inefficiency.
Link to full publication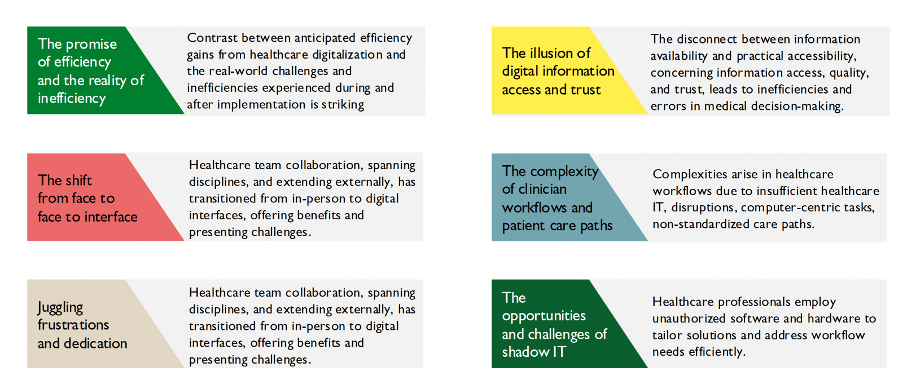
- Practical Recommendations for Navigating Digital Tools in Hospitals: Qualitative Interview Study.
In the interviews, we asked HCPs the question “Based on your experience, what advice would you give to other healthcare professionals who are just starting to use the/digital tool/s?”. Based on their responses, we identified ten key recommendations to help new clinical users effectively navigate digital tools in hospitals. These include taking time to understand the tools, seeking advice from peers, embracing experimentation, and maintaining a human-centered focus. However, ensuring the effective use of healthcare technologies requires a collaborative effort among new clinical end users, healthcare institutions, educators, and regulatory bodies.
Publication coming soon.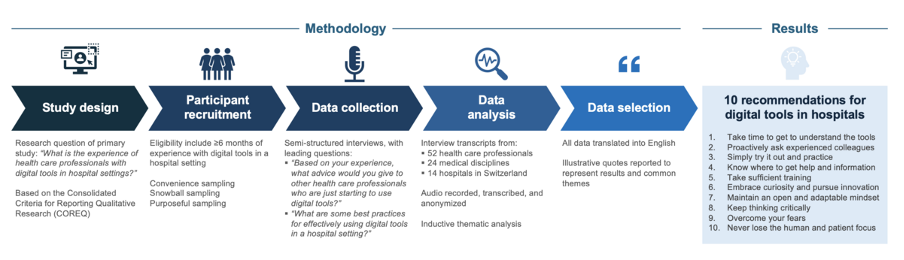
- Applying Large Language Models to Interpret Qualitative Interviews in Healthcare.
We explored the use of LLMs and topic modeling for qualitative data analysis, finding them effective in supporting thematic analysis by automating and enhancing the identification of patterns and topics. While LLMs showed to be promising, the application of LLMs requires careful evaluation to avoid biases and ensure accurate theme integration. However, using LLMs in qualitative data analysis could significantly accelerate the adoption of diverse perspectives in healthcare transformation, fostering a more sustainable and inclusive digital environment.
The paper was presented at the Medical Informatic Europe (MIE) Conference, in Athens, Greece in August 2024.
Link to full publication